Tuberculosis Can Emerge After Cancer Immunotherapy
In December 2012, an 80-year-old man in Florida went to his doctor to have a bulge on his eyelid examined. Tests showed that the bump was a rare form of skin cancer called Merkel cell carcinoma. Despite treatment, the mans cancer spread, first to lymph nodes under his jaw, then to lymph nodes in his abdomen. So in June 2015, he enrolled in a clinical trial for Mercks pembrolizumab (Keytruda), a checkpoint inhibitor drug that blocks programmed cell death protein 1 (PD-1) to help the immune system more effectively target and kill tumor cells.
Six months into receiving the experimental treatment, the man developed an odd-looking nodule in his lung that didnt resemble any of his other tumors. Doctors decided to biopsy it. To their surprise, the results came back positive for tuberculosis (TB), though the man didnt have symptoms of a TB infection. In February 2016, he started anti-TB treatment, and fortunately, after a short break from the anticancer treatment, was able to finish the full courses of both therapies in 2017.
Meanwhile, a second patient, an immigrant from Vietnam, where TB is endemic, had enrolled in a trial for Bristol-Myers Squibbs nivolumab (Opdivo), another anti-PD-1 drug progressing through clinical trials. He didnt have such a happy ending: in June 2016, a month after starting the experimental cancer treatment, he developed a tuberculosis infection. A month after that, he died.
I personally am a little concerned, says Elad Sharon, a medical oncologist at the National Cancer Institute (NCI), which has been one of the government sponsors of clinical trials globally for PD-1 and PD-L1 blockade treatments. Doctors at Emory University, where the Florida man was being treated, alerted the NCI to the mans condition because the agency was responsible for reporting any ill effects of the treatment to the US Food and Drug Administration (FDA). But the mans experience wasnt an isolated case, Sharon says. Reports from other clinical trials of anti-PD-1 treatments also showed tuberculosis infections cropping up in treated patients.
The FDA approved pembrolizumab and nivolumab as therapies for a variety of cancers, starting in 2014. Anti-PD-1 therapies are also being touted as potential treatments for non-cancer diseases such as Alzheimers. Given the enthusiasm to expand these drugs use, combined with the fact that the World Health Organization estimates that nearly a quarter of the worlds population has latent TB, Sharons concern seems justified.
You release the brakes on T cells . . . so TB disease occurs.
Olivier Lambotte, Paris XI University Medical School
This is something that needs a lot more attention, says Dan Barber, an immunobiologist at the National Institute of Allergy and Infectious Diseases (NIAID) who coauthored with Sharon a study describing the two cases of TB after anti-PD-1 therapy (Sci Transl Med, 11:eaat2702, 2019). Those results, and other reports of TB following immunotherapy, suggest that we should probably be thinking about tuberculosis more during trials and during immunotherapy for cancer and actually see if we can try and get a feel for just how likely this is, he says. It could be a very rare event or it could be not so rare. . . . Its not clear.
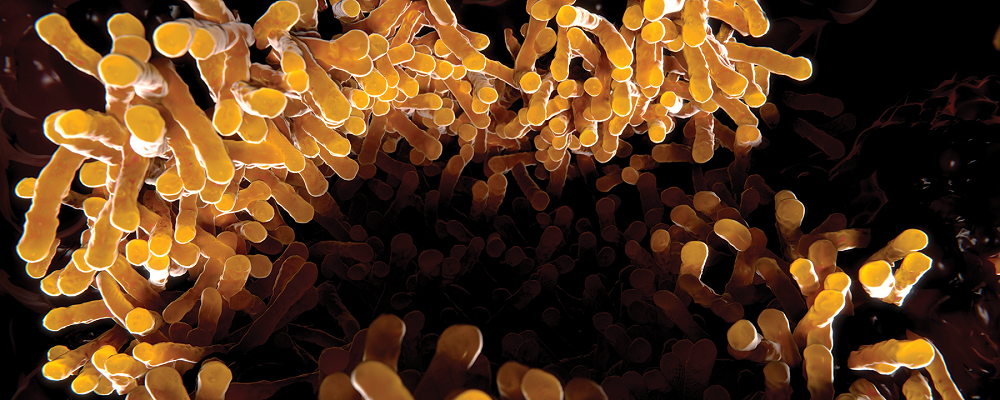
The idea that tuberculosis might emerge after anti-PD-1 isnt a total surprise. In 2010, William Jacobs Jr., a microbiologist at Albert Einstein College of Medicine in New York, and colleagues reported that mice genetically engineered so that they didnt have PD-1 protein surface receptors died extremely quickly compared to healthy mice when infected with the bacterium that causes TB, Mycobacterium tuberculosis (PNAS, 107:13402407). Essentially, Jacobs says, the study showed that the PD-1 pathway was crucial to controlling inflammation that builds in response to the bacterium. Barbers work as a postdoc at NIAID revealed a similar result: after exposure to M. tuberculosis in the air, PD-1 knockout mice developed a lot of M. tuberculosis specific CD4 T cells which play a role in triggering adaptive immune responses and those cells actually encouraged the replication of bacteria in the mice (J Immunol, 186:1598 607, 2011).
In humans treated for cancer who develop TB, the infections are probably not new, but the escape of an old infection kept latent thanks to the PD-1 system, says Olivier Lambotte, an infectious disease researcher at Paris XI University Medical School who has described a case of anti-PD-1 emergent TB but was not involved with Sharons and Barbers work. He explains that PD-1, which is expressed on CD4 T cells, prevents excessive inflammation and immune activation in response to M. tuberculosis. With anti-PD-1 therapy, you release the brakes on T cells . . . so TB disease occurs.
Barber notes that the molecular interactions that lead to illness may be more nuanced. His recent studies in PD-1 knockout mice suggest that CD4 T cells in these animals are making a lot of a cytokine called interferon gamma (PLOS Pathog, 12:e1005667, 2016). Interferon gamma production by CD4 T cells is [the sort of thing] that people think of as being the way the adaptive immune response suppresses tuberculosis, he says. But his work has shown that thats not the case at all. The outcome of boosting interferon gamma production by T cells in a mouse model of TB is a dead mouse. Not better control of the infection.
Up until the Florida patient presented with TB, there werent any data on how the human immune system responded to M. tuberculosis after anti-PD-1 treatment. Samples taken from the mans blood and analyzed by Sharons group, however, showed that interferon gamma producing CD4 T cells specific to M. tuberculosis were indeed more abundant after anti-PD-1 treatment. We were able to really prove, at least to our minds, that the data were consistent with the data that [Barber] had previously put together in the mouse, Sharon says.
Barber, Jacobs, and Lambotte agree that the data suggest that screens for latent TB should be done before a patient undergoes any anti-PD-1 treatment. But Sharon is a bit more hesitant. Were still thinking about it, in part because I think that were just not clear on how common this is, he says, especially when it comes to the severe cases of the patients described in last years Science Translational Medicine study. Clinicians and scientists dont usually monitor for TB in clinical trialsand its possible the nodules that develop from the infection could be mistaken for additional cancer growths.
Still, the results are definitely telling us something unique about the immune response, Jacobs Jr. says. And, it could lead to innovative treatments for TB, perhaps by using anti-PD-1 treatments to encourage persistent M. tuberculosis cells to grow so they can then be killed more quickly by TB drugsan approach that could help reduce the ability of the bacteria to become latent in the body, he explains. Thats an idea I intend to test.